Apps
Definition of Pathological Demand Avoidance
There is no recognised diagnostic definition of Pathological Demand Avoidance (PDA), although it is widely thought of as falling within the Autism Spectrum Disorder umbrella.
Clinicians can currently only use PDA as a descriptive diagnosis alongside an Autism Spectrum Disorder Diagnosis. It is not recognised by either internationally recognised standardised diagnostic tools; the DSM-V or the ICD-11.
Despite the lack of clinically defined diagnostic criteria, it is felt that PDA encompasses those children who are demand and expectations avoidant 'to an extreme extent'. This means the individual becomes highly reactive when demands and expectations are placed upon them by others.
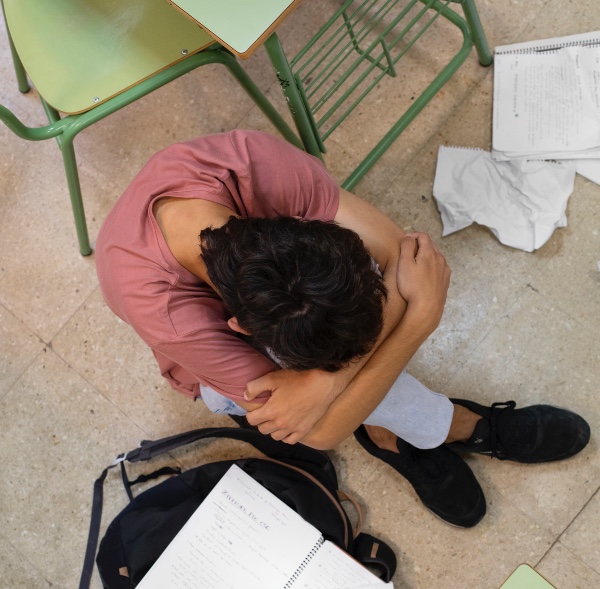
When demands are placed the responses may manifest as extreme demand avoidance and can also develop into a meltdown or panic attack.
Related:
- Read the book: Positive Behaviour Support for Pathological Demand Avoidance
- Online course: Positive Behaviour Support Strategies for Children and Adolescents with Pathological Demand Avoidance (PDA)
- Understanding Pathological Demand Avoidance (PDA) and Anxiety: Strategies for Management and Support
- Positive Behaviour Support for Demand Avoidance Book by Dolly Bhargava
- Ten Effective Classroom Strategies for Teachers Supporting Students with PDA
- Understanding the Differences Between PDA and ODD to provide better support strategies
- Understanding PDA and ADHD - telling the difference
Everyday Features of PDA
Resisting Ordinary Demands: Refusal to comply with even simple or routine requests (e.g., brushing teeth, getting dressed) because it feels overwhelming or intrusive.
Social Strategies to Avoid Compliance: Using distraction, negotiation, excuses, or delay tactics to resist demands. This comes across as being socially manipulative.
High Anxiety Levels: Avoidance behaviours are often driven by acute anxiety.
Obsessive Behaviour: May fixate on particular interests or individuals as a coping mechanism.
Role Play and Pretending: Often use imaginative play or adopt personas to maintain control over situations.

Types of Pathological Demand Avoidance
It is generally agreed that those who fit the profile of PDA are required to first meet the criteria for an Autism diagnosis, alongside the proposed differentiating symptoms of PDA.
Much like with an Autism Spectrum Disorder diagnosis, those who fit the PDA profile present with individualised symptoms which can present differently from person to person.
Defining Demand
Demands can be direct demands such as 'please help wash up' or they can be indirect or implied demand. These indirect requests are harder to identify because they are based on social expectations.
Examples of Indirect or Implied Demands:
Social Expectations: Being expected to join a group activity because "everyone else is doing it" or feeling pressured to conform to unspoken social norms, such as saying "thank you" or making eye contact.
Environmental Cues: A tidy room implying the expectation to keep it clean or a worksheet placed on a desk suggesting it needs to be completed.
Subtle Suggestions: Saying, "It's a nice day for a walk," which might be interpreted as a demand to go outside.
Routine-Based Assumptions: Expecting the individual to follow a routine without explicitly stating it. Anticipating that they will take the same role or responsibility as before.
Why Indirect Demands Matter in PDA
People with PDA often have heightened sensitivity to perceived control and expectations, so even subtle cues can feel like a loss of autonomy. Recognising and reducing indirect demands can help create a less pressurised environment and improve interactions.
There are different types of PDA presentation and the behaviours described will help with identifying pda:
Passive-Avoidant Type
These individuals may initially appear compliant but subtly avoid demands by procrastinating or finding indirect ways to resist. Behaviour includes:
-
Delaying tasks indefinitely (I'll do it later).
-
Becoming withdrawn or unresponsive when demands are made.
-
Often mislabelled as lazy due to their passive avoidance style.
Assertive-Avoidant Type
Resistance is overt and direct, with clear refusal to comply with demands. Behaviour includes:
-
Saying no repeatedly and assertively.
-
Showing anger or frustration when pressured.
-
Using creative excuses or humour to deflect attention.
Socially Manipulative Type
These individuals may use advanced social strategies to avoid demands, demonstrating a high level of social understanding. Behaviours include:
-
Playing on the emotions of others (You're upsetting me by asking that!).
-
Using charm or humour to redirect attention.
-
Manipulating situations to shift control away from authority figures.
Role-Play and Fantasy-Based Type
Avoidance is achieved through imaginative play or pretending to be someone else. Behaviour includes:
-
Adopting personas (e.g., pretending to be a cat that cannot understand human language).
-
Immersing themselves in fantasy worlds to avoid real-world expectations.
-
Dramatically exaggerating situations to justify avoidance.
Meltdown and Shutdown Type
These individuals may experience extreme anxiety leading to emotional meltdowns or shutdowns as a response to overwhelming demands. Behaviour includes:
-
Explosive emotional outbursts (meltdowns).
-
Retreating into a silent, unresponsive state (shutdowns).
-
These behaviours are not deliberate but reflect a loss of control due to anxiety.
Just like Autism itself, PDA presents with a spectrum of behaviours and intensities, varying based on individual traits, sensory sensitivities, and environmental factors. These shared traits might include:
-
Difficulties with social communication abilities or interaction.
-
Restricted interests or repetitive behaviours.
-
Sensory sensitivities.

Causes of Pathological Demand Avoidance
The causes of Pathological Demand Avoidance (PDA) are not yet fully understood, as it is a relatively new and evolving profile within the autism spectrum. Current research suggests a combination of genetic, neurological, and environmental factors may contribute to its development. While the exact mechanisms remain unclear, understanding the potential causes can help inform how we approach and support individuals with PDA.
Neurological and Developmental Factors
Individuals with PDA often exhibit neurological differences that affect how they process everyday demands and social interactions.
Research suggests that heightened sensitivity in areas of the brain associated with anxiety, emotional regulation, and executive functioning could play a role.
Anxiety as a Driving Force
Anxiety is thought to be the primary underlying factor of PDA behaviours. The extreme avoidance of demands arises as a coping mechanism to reduce feelings of being overwhelmed or out of control.
Mental health challenges, such as chronic stress and heightened fight-or-flight responses, are commonly observed in individuals with PDA. This may stem from how their nervous system processes perceived threats, including routine requests.
Social Communication Differences
Unlike classic autism, individuals with PDA often have what appear to be surface social communication abilities. For example, they may come across as socially adept but struggle with deeper, reciprocal social interactions.
This discrepancy between apparent social competence and underlying difficulty can lead to frustration and avoidance behaviours when expectations of social performance feel unmanageable.
Genetic Factors
Like other autism spectrum profiles, PDA is thought to have a genetic component. Studies on autism have identified familial patterns, suggesting a heritable aspect to neurodevelopmental differences.
While no specific gene has been linked to PDA, it is likely that a combination of genetic predispositions contributes to the profile.
Environmental Influences
Early experiences and environmental factors may influence the development of PDA behaviours. For example inconsistent or overly rigid environments may exacerbate anxiety and avoidance tendencies.
Experiences of trauma, heightened stress, or unmet sensory needs in early childhood could contribute to the development of extreme demand avoidance behaviours. A lack of understanding or support for their specific needs can further reinforce the behaviours associated with PDA.
Overlap with Other Conditions
PDA often co-occurs with other conditions, including mental health disorders like anxiety, depression, or obsessive-compulsive disorder (OCD). These overlapping conditions may amplify the individual’s difficulty in managing everyday demands.
Some individuals with PDA may also have other neurodevelopmental disorders, such as ADHD or language processing difficulties, which further impact their ability to cope with expectations.
Evolution of Behavioural Patterns
Over time, individuals with PDA may develop learned behaviours that reinforce demand avoidance. Avoidance strategies like role play or negotiation might become their default response to demands, as they provide a sense of control and reduce immediate anxiety.
These behaviours may be inadvertently reinforced by authority figures who adjust expectations to accommodate avoidance, creating a feedback loop.
The PDA Society and other advocacy groups emphasise the need for further research and awareness to better understand the causes of PDA. They stress that societal misconceptions about demand avoidance can hinder effective support, often leading to misinterpretation of behaviours as oppositional or defiant.
Symptoms of PDA
The proposed diagnostic criterion for PDA is widely debated, however the following symptoms are thought to be demonstrative of a PDA profile:
- Passive early history before the age of 1, avoidant of everyday demands.
- Consistent avoidance of demand and associated panic attacks with this.
- Appear sociable but lack social identity.
- Mood swings and impulsivity.
- Enjoys role play and imaginative play.
- Language delay.
- Obsessive behaviour.
Examples of Demand and Expectation Avoidance Behaviours
The child may use one or more of the following behaviours to resist demands and expectations:
- Becoming argumentative
- Blame others for outcomes
- Bombarding the communication partner with speech or noises to drown out their speech
- Bossy behaviour by constantly telling others what to do
- Changing the topic of conversation
- Complaining of physical ailments
- Constantly negotiating
- Delaying or postponing something
- Distracting the communication partner
- Excuse-making
- Insisting on having the last word
- Interrupting others often
- Mimicking the other’s gestures and/or speech purposefully
- Panic-driven verbal and/or physical aggression
- Physically incapacitating self (e.g., hiding under table, flopping)
- Quick to anger, get upset or worried when under pressure
- Refusing to speak
- Repetitive questioning or talking about the same topic repetitively to avoid doing a task
- Straight-out refusal
- Withdrawing into fantasy world
References
Fidler, Ruth; Christie, Phil (2019). Collaborative Approaches to Learning for Pupils with PDA: Strategies for Education Professionals. Jessica Kingsley Publishers.
Moore, A., 2020. Pathological demand avoidance: What and who are being pathologised and in whose interests?. Global Studies of Childhood, 10(1), pp.39-52.
Newson, E. (2000). Defining criteria for diagnosis of pathological demand avoidance syndrome (2nd revision). Nottingham: The Elizabeth Newson Centre.
Behaviour Help
If you are supporting an individual with this diagnosis, please refer to our services and resources. They aim to help children, adolescents and adults achieve better communication, social, emotional, behavioural and learning outcomes. So whether you are wanting guidance on parenting, teaching, supporting or providing therapy, Behaviour Help is at hand.
Note: This is not an exhaustive list of all the possible causes, symptoms and types but some general information that can be further explored. Based on what you have read if you have any concerns about an individual, please raise them with the individual/s. The caregiver can then raise these concerns with their local doctor who can provide a referral to the relevant professional (e.g. paediatrician, psychologist, psychiatrist, allied health professional and learning specialists) for diagnosis and treatment if appropriate.
Get Started with Behaviour Help App
Assess-manage-prevent behaviours of concern efficiently and effectively with the Behaviour Help App.



